A new study by researchers at University of Limerick has found high rates of anaemia among patients in the health system, while screening for common causes is low.
The research study carried out by a team at University of Limerick School of Medicine found that substantial numbers of men and women in the health system had anaemia, the presence of which is strongly associated with high rates of hospitalisation, death, and poor quality of life.
Anaemia (a low level of haemoglobin in the body) is a common but treatable condition that predicts adverse clinical outcomes. It affects nearly two billion people across the globe and is the third-leading cause of years with lived disability in the world.
While the study revealed a high burden of patients with the condition, it found that there were relatively low rates of screening for treatable causes of anaemia, including deficiencies in vitamin B12, folate, and iron, which highlights an important gap in care delivery programs and emphasises the need for quality improvement initiatives.
Prior to the large population-based study, the prevalence of anaemia and information on its underlying causes was largely unknown as data at the national or regional level was limited.
The research, published in the journal BJGP Open, is the largest study ever to explore the burden of anaemia and the extent of investigation for underlying common causes in Ireland.
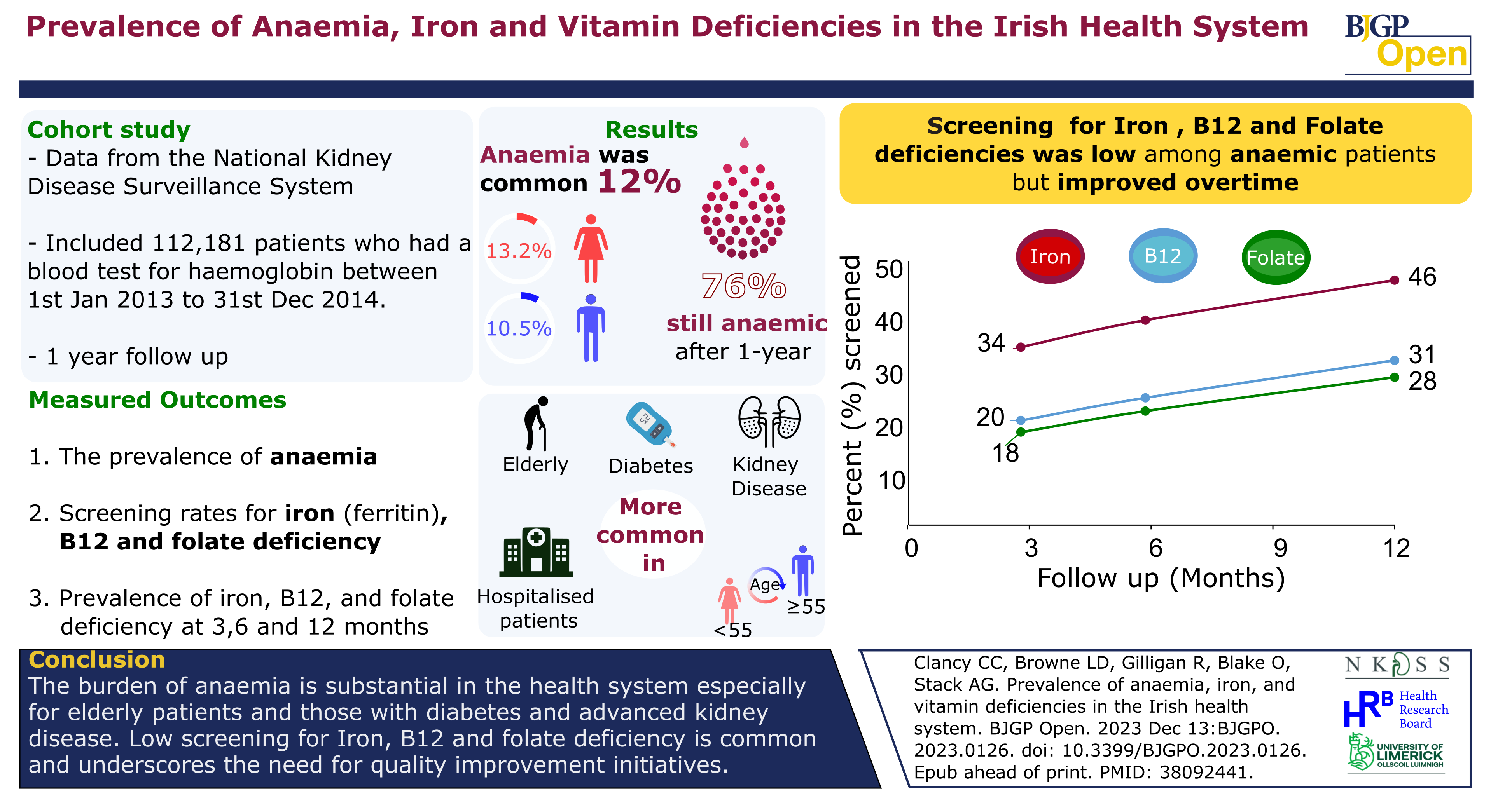
The study found that 12% of Irish patients had anaemia with 1 in 8 women (13.2%) affected and 1 in 10 men (10.5%). Most of these patients were found to have had mild anaemia (9.1% of total), with moderate to severe anaemia present in the remaining 2.9%.
The percentage of patients with anaemia was particularly high in elderly patients, and in patients with underlying medical conditions such as kidney disease, diabetes and for patients undergoing treatment in specific clinical settings.
Despite the high burden of anaemia, less than 20% of anaemic patients were tested for deficiencies of vitamin B12 and folic acid, and only one third of all patients were screened for iron deficiency during follow-up.
Although there was some improvement in screening rates with increasing severity of anaemia, approximately 50% of patients with severe anaemia did not undergo screening.
“This is the largest study to address the magnitude of anaemia and the extent to which it is investigated in the Irish health system,” according to senior investigator Professor Austin Stack, Foundation Chair of Medicine at UL’s School of Medicine and Consultant Nephrologist, University Hospital Limerick.
“Our study reveals a significant burden of anaemia that was present in several high-risk groups, including patients with diabetes, chronic kidney disease, and the elderly. The prevalence of anaemia increased exponentially in older men and women, highlighting their increased vulnerability.
“Patients with advanced kidney disease had nearly eight-fold higher prevalence compared to patients with normal kidney function. Patients who attended the emergency room, outpatient departments or admitted to hospital were found to be particularly affected, with prevalence ranging from 18 % to 29 %,” Professor Stack explained.
Anaemia is a condition in which the body does not have enough healthy red blood cells or haemoglobin (an iron-rich protein) to carry oxygen to the cells around the body.
Haemoglobin is essential for red blood cells to carry oxygen from the lungs to the rest of the body. When someone suffers from anaemia, the body does not get enough oxygen in the blood, and this can cause tiredness, shortness of breath, and dizziness.
The researchers assembled a cohort of 112,181 patients using data from the National Kidney Disease Surveillance System to assess for anaemia and followed them for up to one year to explore the use of screening tests that check for iron deficiency, B12, and folate deficiency.
Co-author Dr Leonard Browne, Senior Research Fellow in Biostatistics at the UL School of Medicine, highlighted the low level of screening for treatable causes of anaemia.
“What is remarkable is that less than 20% of anaemic patients were screened for vitamin B12 and folate deficiency, and only one third were screened for iron deficiency at three-months follow-up,” he explained.
“Despite some improvement with increasing severity of anaemia, approximately 50% of patients with severe anaemia did not undergo screening. Indeed, when we followed patients for up to 12 months, screening rates did increase although modestly for B12 and folate deficiency - 30% - and doubled for iron deficiency - 46%. These findings reveal that common causes of anaemia are inadequately tested for in the wider health system especially among high-risk groups.”
Professor Stack emphasised the importance of screening for and identifying the underlying cause of anaemia.
“We found that one in three patients had evidence of absolute iron deficiency, 6.3% had B12 deficiency, and a further 5.8% were folate deficient. All these deficiencies are easily treated in modern day clinical practice leading to significant improvement in the degree of anaemia. This study provides a valuable starting point from which we can begin to understand practice patterns in care delivery and the development of quality improvement programmes in the health system.
“Iron deficiency is the main cause of anaemia affecting women more than men. The findings from our study correlate well with the international body of evidence, which shows that investigation of anaemia subtype is uncommon and that the standards of anaemia management vary considerably,” Professor Stack added.
The research was funded by the Health Research Board (HRB) and Dr Mairéad O’Driscoll, Chief Executive of the HRB said: “Professor Stack’s research is a really nice example of how intelligent and targeted secondary-data analysis can make important contributions to our knowledge base. The data-driven insights from his work have obvious potential to inform and improve health service delivery.
“The HRB is committed to working with all of our partners to advance the use of primary and secondary data to enhance health policy, to improve healthcare delivery and to drive innovation in our health services.”
The Study “Prevalence of anaemia, iron, and vitamin deficiencies in the health system in the Republic of Ireland: a retrospective cohort study by Conor Clancy and others, has just been published by the [BJGP Open.][https://bjgpopen.org/content/8/2/BJGPO.2023.0126#:~:text=Results%20The%20overall%20prevalence%20of,%25%2C%20P%3C0.001).]