A new study by researchers at University of Limerick has found that control of high blood pressure in adults with chronic kidney disease (CKD) is ‘poor’.
This is significant given that an estimated 400,000 patients in Ireland have chronic kidney disease and that hypertension, or high blood pressure, is a major risk factor for kidney failure, heart attacks and strokes.
The new study by researchers at University of Limerick School of Medicine has just been published in the Clinical Kidney Journal of the European Renal Association.
It is the largest study of its kind to explore the prevalence, awareness and management of hypertension in individuals with kidney disease using data from the Irish Longitudinal Study on Aging (TILDA).
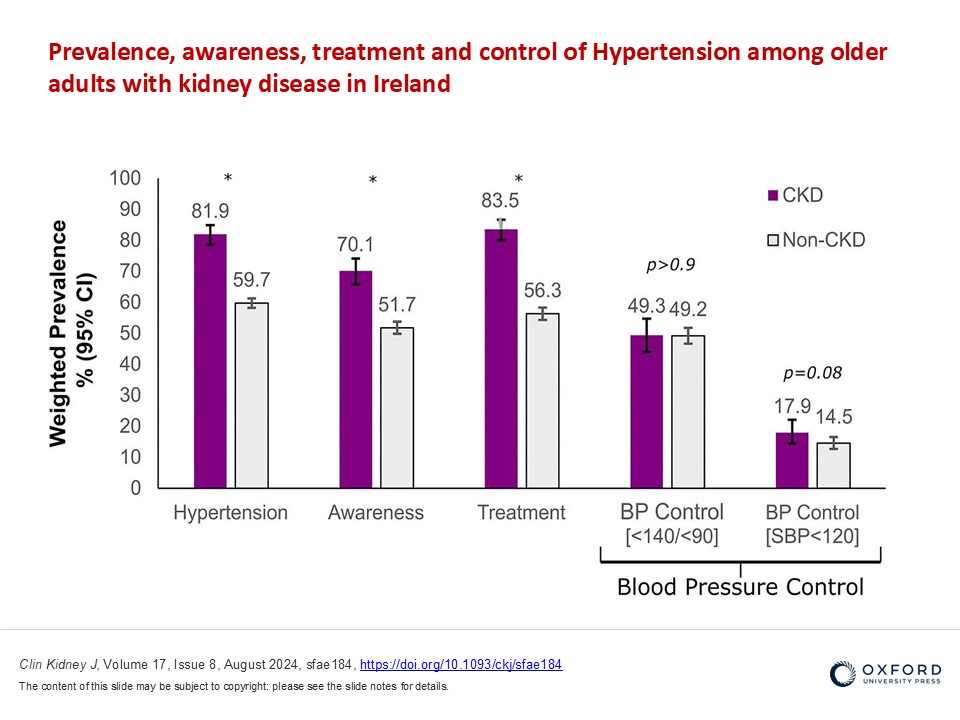
It found that four out of five individuals (82%) with chronic kidney disease in Ireland, age 50 and over, suffer from hypertension, and although the awareness of hypertension and treatment of hypertension are high, control of blood pressure (BP) is far from desired with just under 50% of individuals achieving a desired target.
The study revealed that the burden of hypertension was far more common in individuals with kidney disease than without (81.9% vs 59.7%), especially in men and in older individuals.
The investigators also found that individuals with chronic kidney disease and hypertension were more aware of their hypertension diagnosis than those who did not have kidney disease (70.1 vs 51.7%).
The research further revealed that individuals with hypertension and kidney disease were also more likely to be treated compared to those without kidney disease.
Among the key findings were:
Prevalence of hypertension was extraordinarily high at 81.9% and was much more common than in those without kidney disease Patient awareness of hypertension was far higher in individuals with kidney disease than those without (70.1 vs 51.7%) A large proportion of patients with kidney disease were receiving antihypertensive medications (83.5%) Two thirds of patients with chronic kidney disease were receiving two or more blood pressure medications Blood pressure control was poor with only 49.3% achieving a target < 140/90 mmHg Blood pressure control was even poorer with only 17.9% achieving SBP < 120 mmHg The study was led by Dr Leonard Browne, Senior Research Fellow in Biostatistics, National Kidney Disease Surveillance System (NKDSS) at the UL School of Medicine.
He explained:
“Hypertension is common in individuals with chronic kidney disease and a major risk factor for kidney failure, major cardiovascular events and death. Despite our best efforts using a wide variety of anti-hypertensive medications, achievement of blood pressure control in patients with kidney disease remains a major challenge.
“Our findings are in line with international studies and reveal that while there are high levels of awareness of hypertension, and high rates of treatment compared to individuals without kidney disease, we are not getting patients to desired targets associated with the best outcomes.”
Professor Austin Stack, senior author and Lead Investigator at NKDSS at UL’s School of Medicine and Consultant Nephrologist, University Hospital Limerick, explained: “Unfortunately, the high levels of awareness and treatment did not translate into better blood pressure control. The study shows that less than half of individuals with chronic kidney disease achieved a target blood pressure of 140 over 90, a target that has been set for the majority of patients for many years by the international scientific community.
“The results were markedly worse for individuals aged 75-plus years where the percent dropped to 42.4%.
“Recently, there is evidence to suggest that more stringent control of blood pressure, targeting a lower systolic blood pressure < 120mmHg (rather than 140 mmHg) leads to greater clinical benefit for these patients by reducing further the risk of major cardiovascular events and death.
“However, when we applied this target to our study population, we found that just under 18% of patients achieved this target. Although more stringent blood pressure control may be of benefit to many patients with chronic kidney disease, our data from TILDA with 5,356 individuals suggests that this target is only achievable in less than one in five patients.”
The researchers believe several factors contribute to suboptimal blood pressure control in patients with chronic kidney disease.
Dr Browne noted, ‘Non-adherence to medication is common among many patients, which may partially explain these findings. Additionally, some doctors may hesitate to prescribe additional blood pressure medications due to concerns about overtreatment, higher risk of falls, and ongoing controversy over blood pressure targets.’
“Our findings from TILDA revealed that 62 percent of individuals with hypertension were receiving two or more antihypertensive medications, and this number reached 67% in those age 75 and over. This implies that one third of patients were treated with just a single blood pressure medication leaving much room for improvement. The addition of a second or third antihypertensive medication is often a necessary step in these patients to ensure more effective blood pressure control along with lifestyle modification.
“‘Hypertension is a major risk factor for cardiovascular events in these patients and can be modified with effective therapy. To reduce the risk of kidney failure and major cardiovascular events in Irish patients, we need to improve our management strategies.
“Scientific communities internationally have endorsed lower BP targets of 120 mmHg for patients with kidney disease in order to improve health outcomes and extend life expectancy, while taking into consideration trade-offs between efficacy and safety.”
Dr Angie Brown, Consultant Cardiologist and Medical Director with the Irish Heart Foundation welcomed this study: “In the Irish Heart Foundation, we call high blood pressure the silent killer as most people don’t realise they have high blood pressure unless it is measured.
“This paper demonstrates a significant prevalence of high blood pressure in patients with kidney disease and in particular highlights the importance of the ongoing management of blood pressure as it was found to be high even in patients on blood pressure medication.”
Chief Executive Officer of the Irish Kidney Association, Ms Carol Moore highlighted the impact of this study to the estimated 400,000 patients in Ireland with chronic kidney disease.
“It is very good to see the high rates of patient awareness of hypertension and the high proportion of patients with kidney disease that are receiving treatment. These are steps in the right direction; however, the rates of blood pressure control are less than desired. High blood pressure is a key risk factor for progression into end-stage kidney failure where a patient needs treatment with dialysis or a transplant.
“This not only has a major impact on patient and family lives, but is also an economic burden on the healthcare system, as it costs on average, €125,000 per year, to provide dialysis to a single patient.
“This study really shows that there is a lot more to do. Getting this message out to patients and their healthcare teams is an important goal to improve blood pressure management.”
Professor George Mellotte, Director of the National Renal Office (NRO) and Consultant Nephrologist has signalled the importance of these results and the potential downstream consequences on the growing burden of chronic kidney disease in Ireland.
“We already knew that hypertension is common and severe in patients with kidney disease which leads to higher rates of kidney failure requiring dialysis, and major cardiovascular events like heart attacks and strokes. Better control of blood pressure will reduce these risks and prevent a considerable amount of suffering.
“The introduction of quality improvement programmes such as the Chronic Disease Management Programme (CDM) should lead to higher levels of awareness of hypertension, better treatment outcomes and less chronic kidney disease, and more patients avoiding dialysis or kidney transplantation.”
The research was funded by the Health Research Board (HRB) and Dr Mairéad O’Driscoll, Chief Executive of the HRB said: “The HRB invests in secondary data analysis projects (SDAPs) because they help to deliver advances in health policy and practice, as demonstrated by this research by UL’s School of Medicine.
“Since 2021 the HRB has invested €7 million in this area and it is clearly delivering results. We plan to launch another funding opportunity for SDAPs in 2025.
“The findings illustrate the important role that accessible datasets play in empowering researchers to make important discoveries, while also protecting the privacy and confidentiality of study participants.”
The study, ‘Prevalence, awareness, treatment, and control of hypertension in community dwelling older adults with chronic kidney disease: the Irish longitudinal study on ageing by Leonard D Browne, Austin G Stack and others, has just been published by the Clinical Kidney Journal.